Impingement Syndrome
Are you experiencing shoulder pain? Impingement syndrome typically is characterized by weakness, difficulty lifting objects and pain when lying down. Obtaining an accurate diagnosis of the source of the pain is important in receiving proper treatment that will provide long-term relief. At Nebraska Hand & Shoulder, we specialize in diagnosing and treating shoulder pain. Make an appointment today so you can stop living with shoulder pain and start enjoying life again.
Understanding Impingement Syndrome
Pain about the shoulder is one of the most common reasons for a visit to an orthopedist. Except for recurrent dislocation, most shoulder problems occur after age 30. Pain originating in the shoulder must be differentiated from pain referred from other sources such as degenerative intervertebral discs in the neck, heart attack, or carpal tunnel syndrome.
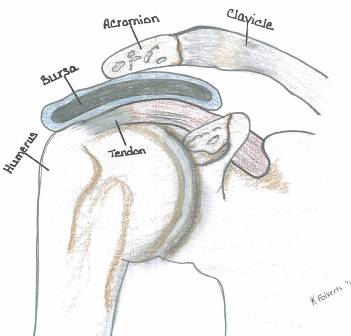
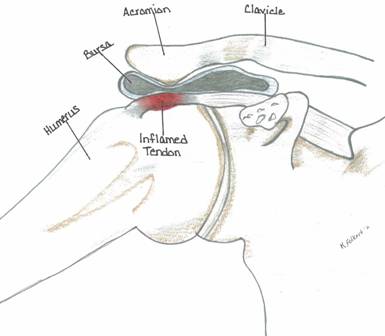
Impingement syndrome is pain related to rubbing of the rotator cuff tendon and/or biceps tendon against the overlying acromion.
Normal Acromion
Prominent Acromion

Normal Acromion (Type 1)

Prominent Type 3 Acromion
Impingement Process and Acromion Types
An impingement process tends to occur in several ways:
A very prominent acromion; typically it is a type 2 or type 3. People with a flat type 1 acromion rarely see an orthopedist for shoulder pain.
As the person ages, the acromion will often enlarge where it attached to the coracoacromial ligament. The acromion seems to follow the course of this ligament downwards, forward and towards the midline of the chest. Thus, we are more likely to see a very prominent acromion in an older individual. Arthritis of the acromioclavicular joint is very common at an early stage at age 40 and older. The majority of people are completely without symptoms (asymptomatic). As degenerative arthritis progresses the joint enlarges; this is true anywhere in the body. In the shoulder, you can feel it when you run your hand over the top of the shoulder as a lump.
The same amount of prominence projects downward and that is what can rub on the rotator cuff very close to where the tendon comes off the muscle at the edge of the glenohumeral joint. Impingement can be affected in a very small percentage of people by posture. The scapula rotates over the humeral head. If one has their shoulders “scrunched up”, pointed towards the breastbone, the acromion may well be relatively more prominent over the rotator cuff. When examining a person with this situation, the shoulder blades are really separated widely on the backside. This is referred to as scapular dyskinesia, a concept popularized by Ben Kibler, MD, of Kentucky. It is very hard to overcome this dysfunctional motion and the associated complaints that come from it. Concentrate on good posture with shoulders back and head held high.
Anatomy
The shoulder is one of the most complex and active joints in the body. The shoulder is suspended off of the chest wall by the shoulder blade (scapula) and surrounding muscles. The shoulder has two true joints: the acromioclavicular (AC) and the glenohumeral as well as a sort of pseudo joint between the shoulder blade and the chest wall. The glenohumeral joint gets its stability from a combination of muscles. Four of the muscles compromise the rotator cuff. These muscles include the supraspinatus, infraspinatus, teres minor and subscapularis. They are responsible for some of the motion of the glenohumeral joint and for stabilizing the joint. Loss of the equilibrium of these muscles and stabilizing forces of them may lead to painful impingement. Variations in normal anatomy are largely responsible for the bulk of non-injury related shoulder pain.
Cause
Age related changes in the shape and prominence of the skeleton of the shoulder, degeneration of the supraspinatus tendon (top portion of the rotator cuff) and changes in physical fitness are probably responsible for the majority of symptoms. Onset of pain follows from this spontaneous process.
Impingement relates to pressure against the rotator cuff resulting in pain. Impingement syndrome has been linked very closely to one of several situations. Elongation of the front edge of the acromion occurs as the coracoacromial (CA) ligament calcifies with age. This may account for the age related higher incidence of impingement syndrome. Most people presenting with impingement syndrome are over the age of 30 though it is occasionally seen in teenagers.
Lack of good muscle tone, muscle imbalance, or fatigue of the muscle may result in the shoulder shifting into such a position where the rotator cuff and the overlying subacromial bursa are impinged upon by the acromion and the CA ligament due to dynamic instability. True instability related impingement syndrome is a difficult diagnosis to make. It is a diagnosis of exclusion, meaning other sources of discomfort have been ruled out first. This is most often seen in throwing athletes with hyper-mobile joints.
It's difficult to discern whether a person has bursitis vs. tendonitis because the bursa sits right upon the rotator cuff tendon. From a practical standpoint, treatment for one results in treatment of the other and, therefore, it's not worth arguing over the small distinction. Because there is only a small space (small tolerances) for the rotator cuff in the subacromial space, loss of stability through fatigue, ligament stretching, or muscle imbalance with or without prominent acromial bone results in pinching of the bursa by the CA ligament and the acromion.
Symptoms of Impingement
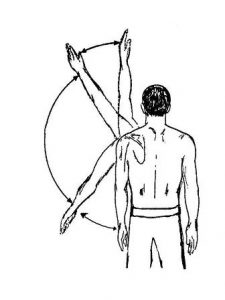
Pain often occurs when lying down and especially with motion of the shoulder from about 60-120 degrees forward and to the side.
Weakness and difficulty lifting things due to pain.
Symptoms of AC Arthritis
Pain from 120 to 180 degrees of abduction.
Pain at the top of the shoulder.
What the Doctor Notes During Exam
Decreased range of motion
Localized tenderness
Guarding/hesitation on active motion
Relief of pain with injection of local anesthetic
Diagnosis
Careful examination in conjunction with a history of onset of symptoms are the most important in making a diagnosis. X-rays are very useful in ruling out fracture and in assessing the shape of the acromion. X-rays are also important in surveying for the presence of arthritis. This is done by looking for increased density of the bone (sclerosis), narrowing of the joint space or extra bone formation (spurs/osteophytes), and excluding the presence of calcified tendon deposits. If symptoms fail to respond to medication or exercise, then it's important to perform an arthrogram. This simple test is performed by sterilely injecting contrast medium into the shoulder joint under local anesthesia. We look to see if contrast leaks out of the normally completely enclosed joint space. MRI scanning is rarely as useful as an arthrogram because it's difficult to discern inflammation of the rotator cuff tendons from a tear; MRI also costs 3x as much. MRI may be useful in the unusual event of a recurrent rupture of the rotator cuff.
Unfortunately many people in the age group with symptoms of impingement have multiple degenerative processes simultaneously such as arthritis of the neck or a pinched nerve making isolation of the problem and solutions to or even improving these pain syndromes difficult. Sometimes the problem is narrowed down by the process of elimination by treating each of the separate entities.
Treatment
Initial treatment for rotator cuff impingement tendonitis depends upon the severity of the symptoms. For someone experiencing moderate to severe pain and associated limitation of motion, corticosteroid injection into the subacromial space is usually a pain free method of getting rapid resolution of the irritation. This is much akin to pouring water on a fire. If there is enough inflammation and depending upon the amount of the prominent bone impinging upon the tendon, it may be necessary to give a couple of injections over the course of a few weeks. This is frequently supplemented by the use of oral, nonsteroidal anti-inflammatory medications (NSAID). This combination is effective in about 7 out of 10 patients.
Surgical Solution - Acromioplasty
If pain persists, affecting one's job or prevents one from sleeping at night, then after a few months of failed treatment, an outpatient should consider minimally invasive surgery. This surgery could solve the problem. Dr. Ichtertz has extensive experience in performing arthroscopic surgery of the shoulder. The inside of the shoulder is viewed with a fiberoptic scope through small puncture wounds. Then the prominent bone is trimmed as are other damaged tissues. The outer clavicle at the AC joint needs trimming in about 40% of the cases. This minimizes discomfort and frequently allows the doctor to do surgery without putting any absolute restrictions on a patient's activities afterwards. Recuperation from the initial surgery is quick with return to work in under a week. Usually, about 3-6 months are allowed for a person to reach their endpoint with full or almost full motion and minimal to no residual pain.

Torn Rotator Cuff Tendon
In the event that the rotator cuff has frayed through and ruptured, it is usually necessary to excise the damaged, degenerative portion of the tendon and reattach it to bone. This precludes active flexion (forward elevation) and abduction (elevation away from one's side) of the shoulder for about 4-6 weeks. Heavy lifting should be avoided for up to 3 months.
Labral Tears
The glenoid (socket) is flat. The labrum acts as a flexible retaining wall helping to maintain the humeral head in a stable position with the glenoid. Shear stresses and age probably account for most labral tears. It's difficult to tell the extent of symptoms developed from a torn labrum rather than the impingement process (acromion jams into cuff). Due to the potential pain contribution, labral tears were usually trimmed or repaired by an anchor to eliminate this source of pain. Impingement is relieved with acromioplasty at the same time.
Labral tears are fairly rare overall. The results of repair of the labral tear are unpredictable. Most agree that repairing them in persons older than about 40 years old is prognostically bad with the people ending up with a lot of stiffness. Dr. Ichtertz believes the trend now is to cut the biceps tendon just off of the labrum and secure it to the upper end of the humerus bone, i.e. biceps tenodesis. By doing this the biceps tendon is no longer pulling on the labrum. It has been reported by Paschal Boileau, MD, a well-respected shoulder surgeon, that he has done this in a large series of patients including Olympic competitors without treating the labrum, just the biceps, and the patients did fine.
Biceps tenotomy, an alternative to biceps tenodesis, has a tendency to result in some residual weakness, perhaps 10-20%, but somewhere between 20-40% of the people undergoing this procedure will continue to have some aching in the shoulder in addition to a deformity from the shortened muscle (Popeye muscle). Tenotomy is much easier than tenodesis for the surgeon, but one has to weigh the odds. Dr. Ichtertz is in favor of biceps tenodesis in the appropriate patient. Rarely would he recommend a tenotomy based upon the relative ease over tenodesis and the potential side effects of tenotomy.
The ideal patient for a biceps tenotomy according to Paschal Boileau, MD, is a patient with a non-repairable rotator cuff tear who maintains good mobility. The worst indication for a biceps tenotomy would be someone with pseudoparalysis of the shoulder with a near irrepairable rotator cuff tear.

Above are MRI images of labral tears. The arrows in each image are pointing to where the dye has leaked into the labral tear.
WARNING: MAY CONTAIN GRAPHIC IMAGES
Frozen Shoulder
While undergoing treatment with medication, it is important to make sure that you maintain as much motion as possible to prevent a frozen shoulder (aka adhesive capsulitis). This is a painful situation wherein the capsule of the shoulder tightens up, restricting motion. In order to maintain motion, it may be necessary to have you seen by a physical therapist for gentle passive and active assisted range of motion in association with application of hot packs and/or ice. The exercise can also be done at home but it's sometimes hard to get family members to get involved in painful situations. Severe contracture requires stretching the shoulder under general anesthesia, so don't let it occur in the first place!
Calcific Tendonitis
If a person presents with calcific tendonitis, cortizone injection usually rapidly resolves the problem. It is recommended that the medication be injected directly into the rotator cuff in the area of the calcification (supraspinatus tendon). While recuperating, frequent overhead reaching, grasping, throwing and circumduction motion such as washing a car, etc. are discouraged because of their exacerbating effect on the impingement process. This diagnosis almost always excludes a torn rotator cuff.
Post-Op Synopsis for Impingement (Rotator Cuff Intact)
- On 3rd post-op day return to work as tolerated
- Physical therapy if full motion has not been obtained within 2-3 weeks of surgery
- Anticipate maximum medical improvement 3-6 months after surgery
Sports
The general principle of being released back to sports is it’s best to resume the game slowly and progressively. A range of motion exercises should precede your game. Limit play time initially, then slowly increase the intensity and duration of your game. In some sports, i.e., tennis, overhead swinging may be avoided.
Swimming: Breast or side stroke may come more easily than front crawl or butterfly strokes. Backstroke may be well tolerated. Consider alternating your swimming style.
Throwing Sports: Start with easy throwing then gradually increase to harder throwing. Try to maintain a smooth throwing motion that will make use of the overall strength of your body.

Results
Results of surgical treatment depend upon age, activity level, occupation, or non-occupation causation and associated degenerative conditions such as cervical degenerative disc disease. Overall, studies have shown that about 85% of people get a very good result after treatment for impingement or a torn rotator cuff. Time from the onset of symptoms to treatment may be important especially for a torn rotator cuff (best if repaired within 3 weeks of tear). In some cases impingement syndrome seems to cause tearing of the rotator cuff, thus, intervention for impingement may also be preventing a torn rotator cuff.
Bigliani LH, Morrison DS, April EW: The morphology of the acromion and its relationship to rotator cuff tears. Ortho Transactions, 1986;10:228.
Burkhead Jr, WZ: The Biceps Tendon. (Philadelphia, PA: Saunders, 1990. The Shoulder, Chpt 20, pp. 791-836).
Calvert PT, et. al.: Arthrography of the shoulder after operative repair of the torn rotator cuff. J Bone & Joint Surg, 1986;68B 1:147-150.
Crymble, B. “Brachial Neuralgia and the Carpal Tunnel Syndrome.” British Journal of Medicine, Vol. 3, 470-451, 1968.
Edelson JG, Taitz C: Anatomy of the coraco-acromial arch; relation to degeneration of the acromion. J Bone & Joint Surg, 1992;74B-4:589-594.
Edelson JG: The ‘hooked’ acromion revisited. J Bone & Joint Surg, 1955;77B-2:284-287.
Gartsman G: Arthroscopic acromioplasty for lesions of the rotator cuff. J Bone & Joint Surg, 1990;72A-2:169-180
Ha’eri G, et. al.: Shoulder impingement syndrome: results of operative release. Clinical Ortho & Related Research, 1982;168:128-132.
Kummel BM, Zazanis GA: Shoulder pain as a presenting complaint in carpal tunnel syndrome. Clinical Ortho & Related Research, 1973;92:227-230.
LaBan, Myron M., Zemenick, GA, and Meerschaert, JR. “Neck and Shoulder Pain: Presenting Symptoms of Carpal Tunnel Syndrome.” Michigan Medicine, September 1975, pages 449-450.
Matsen FA III, Harntz C: Subacromial impingement. (Philadelphia, PA: Saunders 1990. The Shoulder, Chpt 15, pp. 623-246).
MRI of rotator cuff tears. MR Insights (Orange, CA: Alliance Imaging, Inc.), Vol. 4, No. 3, Fall 1994.
Neer CS II: Impingement lesions. Clinical Ortho & Related Research,1983;173:70-77.
Neer CS II: Anterior acromioplasty for chronic impingement syndrome in the shoulder: a preliminary report. J Bone & Joint Surg, 1972;54A:41.
Nirschl RP: Rotator cuff tendonitis: basic concepts of pathoetiology. AAOS Instructional Course Lect., 1989;38:439-445.
Post M, Cohen J: Imipingement syndrome: a review of late stage II and early stage III lesions. Clinical Ortho & Related Research, 1986;207:126-132.
Rathbun JB, Macnab I: The microvascular pattern of the rotator cuff. J Bone & Joint Surg, 1970;52B-3:540-553.
Shoulder pain: rotator cuff tears. Magnetic Resonance Update (Santa Cruz, CA: Dominican MRI Center) 1989.
Tibone JE, Jobe FW, Kerlan RK, et. al.: Shoulder impingement syndrome in athletes treated by anterior acromioplasty. Clinical Ortho & Related Research, 1985;198:134-140.
Shoulder Pain From Nerve Entrapment (i.e. Carpal or Cubital Tunnel Syndrome)
Crymble, B. “Brachial Neuralgia and the Carpal Tunnel Syndrome.” British Journal of Medicine, Vol. 3, 470-451, 1968.
Kummel BM, Zazanis GA: Shoulder pain as a presenting complaint in carpal tunnel syndrome. Clinical Ortho & Related Research, 1973;92:227-230.
LaBan, Myron M., Zemenick, GA, and Meerschaert, JR. “Neck and Shoulder Pain: Presenting Symptoms of Carpal Tunnel Syndrome.” Michigan Medicine, September 1975, pages 449-450.