Cubital Tunnel Syndrome
People with cubital tunnel syndrome often notice a numbness or burning sensation in the outside of their hand that radiates from the elbow to the hand. If you are waking up at night with pain in your forearm, you may be worsening this condition by sleeping with bent elbows. This condition is caused by pressure that is put on a nerve that runs the length of your arm all the way down to your fingers. This is especially common in people who have carpal tunnel syndrome.
There are 3-man surgical treatments for cubital tunnel syndrome. At Nebraska Hand & Shoulder, our surgical solutions allow our patients the shortest amount of recovery time and are usually handled through outpatient surgery. Additionally, using advanced techniques, Dr. Ichtertz is able to minimize scarring while providing excellent results for his patients.
It's important to be treated for this condition as soon as possible as it can cause permanent degenerative conditions which are irreversible when left untreated.
New-onset ulnar symptoms after carpal tunnel release
It's not uncommon to have patients experience numbness, tingling or burning in the pinky, ring finger or side of the hand after carpal tunnel surgery. Usually, the person can be informed to expect this if they are carefully examined, including thorough nerve conduction studies preoperatively. People tend to focus on what they are noticing the most; i.e. who is talking the loudest, the squeaky hinge, etc. thus, they tend to be very aware of the symptoms of the carpal tunnel which is the "eyes" of the hand - the thumb, index, and long fingers for dexterity. Only after those symptoms are eliminated with carpal tunnel release they will become aware of the less noticeable decreased sensibility in the ulnar side of the hand. Aside from the sensory symptoms in the fingers in the ulnar side of the hand, clumsiness, aching in the hand or forearm, and sometimes even the aching or numbness radiating up to the shoulder and neck in addition to awakening at night due to your hands may be experienced with either a pinched median nerve or a pinched ulnar nerve.
Weakness may occur due to the ulnar nerve being compressed while carpal tunnel syndrome does not cause true weakness.
Pressure-Specific Sensory Device (PSSD)
In 2002 Dr. Ichtertz visited with A. Lee Dellon, M.D., Professor of Plastic Surgery and Neurosurgery at Johns Hopkins University Medical Center and author of over 250 scientific articles. The goal was to gain a full understanding of the technique and application of quantitative sensory examinations using the NMT Pressure-Specific Sensory Device (PSSD) which had been developed and studied in the diagnosis of peripheral neuropathy - most specifically diabetic peripheral entrapment neuropathy and FDA approved. Dr. Ichtertz added this to his clinical armamentarium and has utilized the technology to further enhance the diagnosis and improve the treatment of ulnar nerve entrapment, both nonoperative and operative - specifically cubital tunnel syndrome.

Key Pinch

PSSD in Use

Misdiagnosis of Cubital Tunnel Syndrome
The most common misdiagnosis of this overlooked problem is carpal tunnel syndrome. The second most frequent misdiagnosis for cubital tunnel syndrome is an incorrect diagnosis of thoracic outlet syndrome (TOS).
What is Thoracic Outlet Syndrome?
Thoracic outlet syndrome is an extremely rare condition known as a diagnosis of exclusion, meaning that there is no way of proving it is present. Any other diagnosis that the person may have that explains the symptoms is more likely to be the cause than TOS and must be ruled out. Thoracic outlet was the original diagnosis ascribed to anyone with what ultimately turned out to be carpal tunnel syndrome in the early 1900's before a good understanding of nerve entrapment had been developed and before the advent of nerve conduction studies.
Thoracic Outlet Syndrome Treatment
The treatment for confirmed thoracic outlet syndrome is the removal of the patient's 1st rib. Removal of the 1st rib takes the tension off of the entire C8 and T1 roots. These roots ultimately contribute all the fibers to the ulnar nerve. Thus, it is possible to decrease or eliminate cubital tunnel symptoms by decreasing the tension on the ulnar nerve at the cubital tunnel indirectly by taking out a person's 1st rib. Symptoms are usually solved by releasing the pressure on the ulnar nerve at the cubital tunnel of the elbow. Thoracic outlet syndrome is very rare, especially when patients are carefully scrutinized for the presence of cubital tunnel syndrome which will account for the majority of patients who are incorrectly diagnosed with TOS.
The cause of cubital tunnel syndrome is almost exclusively prolonged - but not repetitious - elbow flexion.




Examples of how NOT to sleep. The elbows should be straight.
Negative Effects of Elbow Flexing
Studies beginning in the 1950s (see references) confirm that flexing the elbow beyond 40 degrees puts tension and pressure on the ulnar nerve behind the medial epicondyle of the elbow; while the space at the elbow for the nerve in the retrocondylar groove (cubital tunnel) diminishes as the tension increases in the elbow with further flexion.
The most eloquent paper on this topic was published by Seror in the Journal of Bone and Joint Surgery, British Edition, 1992. However, Dr. Dellon at Johns Hopkins has reported the most detailed analysis of a large series of patients. Maximum tension and pressure on the nerve occur when the person's shoulder is elevated away from the body, elbow flexed fully, hands above the head. This position is demonstrated by a person sitting or lying with her hands above their head, elbows flexed, or lying face down with an arm above the head, elbow flexed.
Eliminate Symptoms of Cubital Tunnel Syndrome
Often patients who present with cubital tunnel sit in the office exhibiting this very same maladaptive posture! Multiple researchers have proven that prevention of this posture by use of an elbow splint at night to hold the elbow straight and to gain the cooperation of the patient has about a 7 out of 10 chance of eliminating the symptoms of cubital tunnel syndrome if a person is cooperative and if they present before irreversible nerve damage has occurred. The remaining 3 out of 10 people will go on to require surgical decompression of the ulnar nerve with an expectation of a good to excellent result in 85-90% of the people as long as they don't have muscle wasting at the time of presentation.
Abnormal Artery and Anconeus Epitrochlearis Muscle
Dr. Ichtertz has identified a previously unknown cause of cubital tunnel syndrome, that of an abnormal artery pressing the nerve as it exits out of the cubital tunnel proper into the flexor carpi ulnaris muscle. The artery is actually just beneath the origin of the muscle.
An abnormal muscle has been identified in a variable number of people known as the anconeus epitrochlearis muscle. When this muscle is present, a tight band that is usually directly over the nerve, or arcuate ligament, is usually absent. I believe that the muscle itself may tightly bind the nerve, though this is uncertain. In patients with cubital tunnels with anconeus epitrochlearis, the muscle is released as part of the procedure. It just changes the operative exposure a little bit; nothing else changes.
It is believed that about 1/3 of the patients who have bad enough cubital tunnel syndrome to go on to require surgery will have normal nerve conduction studies because of the limitations in our ability to test the nerves. Generally it is considered that only 5-10% of most patients presenting with carpal tunnel syndrome are not going to be able to be confirmed to have entrapped nerves on nerve conduction study using the best electrodiagnostic technique and equipment.

This image depicts that with the elbow straight, the ulnar nerve is not compressed or stretched.

Elbow brace used in the nonoperative treatment of cubital tunnel syndrome.
WARNING: MAY CONTAIN GRAPHIC IMAGES

Inability to pinch with thumb straight is Froment's sign.

Diagnosis of Cubital Tunnel Syndrome
The diagnosis of cubital tunnel syndrome is dependent on a keen awareness of it as a possible cause of symptoms and careful clinical examination (local squeezing of the nerve for signs of tenderness, or tingling or burning radiating down into the ulnar side of the hand and forearm), the elbow flexion test which temporarily increases the pressure of the nerve, assessment for weakness of pinch, weakness or decreased ability to abduct and adduct - draw together or place apart the fingers, and in a more advanced case a positive Froment or positive Wartenberg sign which generally would be considered to have a poor prognosis because of the evident muscle wasting that is usually occurring simultaneously. Clawing of the hand is a late and usually essentially irreversible manifestation of untreated, late to present cubital tunnel syndrome.
Variations in Presentation of Cubital Tunnel Syndrome

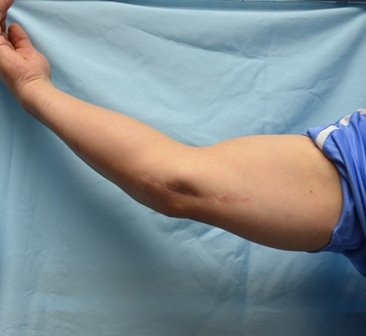
A cubital tunnel patient in 2006 with no muscle wasting in either hand.

The same patient in 2011 with muscle wasting beginning in the left hand. The right hand is still normal.

A patient with severe muscle wasting of the intrinsic hand muscles (small muscles between the metacarpal bones).

A patient with muscle wasting and the red arrow is indicating clawing of the hand (essentially irreversible manifestation of untreated, late to present cubital tunnel).
Do You Need Surgery?
Surgery for cubital tunnel syndrome is necessary with ongoing symptoms and should be offered in short order to somebody who presents with obvious weakness of pinch and/or grips with demonstrated nerve conduction anomaly confirming nerve entrapment at the cubital tunnel because of the poor prognosis for late treatment of this entity. Additionally, if a person has ongoing symptoms in the absence of weakness, she should still be given the option of surgical decompression if she is unable or unwilling to comply with elbow extension splinting at nighttime. A rare person who fails to benefit from elbow splinting and swears to comply with that means of treatment is noted to have a congenital anomaly which has led to the ulnar nerve entrapment.
Occasionally a childhood injury resulting in a broken elbow (supracondylar humerus fracture) will heal with angular deformity.
This has been much less common in the last 15-20 years because of more aggressive surgical intervention for improved outcome. Angular deformity may cause greater tension on the ulnar nerve at the elbow.

X-ray of a normal elbow. Normal is around 15 degrees.

X-ray of angular deformity (35-40 degrees) after a fracture. This puts pressure on the ulnar nerve at the elbow.

X-Ray of Fractured Elbow Before Alignment

X-Ray of Fracture aligned and held with pins
Cause of Cubital Tunnel Syndrome Symptoms Are Unclear
It is unclear what contribution vigorous forceful muscle activity in the upper extremity such as a laborer might contribute to the development of or ongoing symptoms of cubital tunnel syndrome. People who are more physically active at the time of presenting with carpal and cubital tunnel syndrome will tend to complain of more symptoms. It is unclear whether that is in any way actually worsening the problem rather than just making the person aware of the underlying problem. This to a large extent is what is construed as occupational aggravation of the problem under worker's compensation for a minority of patients presenting with either carpal or cubital tunnel syndrome.
The research done on entrapment neuropathy, particularly that not funded by groups primarily benefiting from the outcome of that research; i.e. people receiving multiple NIH grants, etc., tend to suggest that the majority of entrapment neuropathy is age and genetics and possibly general health-related (age over 30, female rate of presentation 2-3 women per men, strong family histories frequently obtainable, much higher rate in diabetics and in the obese). There is no direct link to any occupation with the exception of sorting diamonds or working under a microscope or holding a telephone receiver on a prolonged basis for the development of cubital tunnel syndrome.
Medial Epicondylitis
Medial epicondylitis or "golfer's elbow" is a degenerative condition of the flexor muscle origin in the "medical epicondyle" of the humerus of the elbow. The majority of people presenting with inner elbow pain, however, do not have "medial epicondylitis" which actually implies an inflammatory condition, but they are experiencing the manifestation of entrapment of the ulnar nerve at the cubital tunnel; i.e. a variation in cubital tunnel syndrome. This was proven in research published by Morey and Gabel at the Mayo Clinic. I have verified this also with NCS and Pressure-Specific Sensory Device tests. Medial epicondylalgia (pain at the inner elbow) is the best terminology applied to this until an absolute diagnosis is confirmed by nerve conduction studies. Medial epicondylosis is best treated by corticosteroid injection and avoidance of pressure on the inner elbow along with making certain that the person is sleeping with her elbows extended (straight). Ultimately failure to respond to nonoperative treatment benefits from medical epicondyle removal (medial epicondylectomy), at which time formal ulnar nerve decompression can be carried out to ensure that the symptoms are completely eliminated.
WARNING: MAY CONTAIN GRAPHIC IMAGES
Operative Treatment of Cubital Tunnel Syndrome
Over the years, about seven different operations have been reported and discussed in medical literature regarding surgical treatment of cubital tunnel syndrome. Learmonth, who in my opinion has had a great influence on the misdiagnosis of carpal tunnel syndrome as TOS historically was also the early proponent for submuscular transposition; i.e. moving the ulnar nerve beneath the muscle bed, bringing it away from the inner side of the elbow and away from the stretching and compressing that would occur there. This is probably one of the least performed procedures because it is so aggressive and invasive, and takes so long to heal with weeks off of work and in most hands a large surgical scar. There has been no proven added benefit.
Techniques
In-situ decompression of the ulnar nerve at the elbow is a technique wherein the arcuate ligament directly upon the ulnar nerve is simply released. This has gained a lot of press in the last few years without long-term follow-up. Endoscopic cubital tunnel release was introduced about 1995 by Dr. Tsai at the Kleinert clinic. While his technique has been met with resistance the concept has gained momentum recently. Traditional cubital tunnel surgical options have often left unsightly scars. Depending upon the technique used by each surgeon substantial temporary limitations have also been imposed. For the few of us using science as our guide immediate activity with almost no restriction has been possible. This includes a minimal incision size made possible by operating under magnification.
Two elements appear to be involved in ulnar nerve entrapment at the elbow: a) compression behind the arcuate ligament especially upon bending (flexing) the elbow and b) stretching of the ulnar nerve that also occurs upon elbow flexion. Thus the worst posture a person might assume is face down (prone) while sleeping.
6-inch Incision vs. 3/4-inch Incision - Which Would You Prefer?
Submuscular transposition surgery causes a large, unnecessary scar along the elbow.

Endoscopic cubital tunnel release results in a small, 1.5-2 cm incision along the elbow.
Limited Reports of Success
Only limited reports of successful surgery done in-situ, i.e. decompressing the nerve while leaving it lying in its original position, were available until recently. Those of us determined to achieve the best results have held off on using an in-situ approach fearing poor results because the band compressing the nerve is addressed but not the ongoing problem with stretch. The concern over this has recently been reduced. Dr. Reimer Hoffmann of Germany in a large series The Endoscopic Management of Cubital Tunnel Syndrome. M.Siemionow has demonstrated fine results using his endoscopic approach with facial plastic surgical tools and a fiberoptic scope in over 700 patients in all states of disease from mild to severe. Though not offering convincing data, several other surgeons have been advocating an in-situ approach for years. Only Dr Hoffmann has the data and the truly in-situ technique to back it up. However, the highest failure rate has been reported Washington University of 19% using an in-situ release. This may be because of continual poor sleep positions that continue to stretch the ulnar nerve.
Low Recurrence Rates
Cubital tunnel syndrome has an extremely low recurrence rate once operatively treated. It is so small it has not been accurately determined. Before declaring a person has recurrence of cubital tunnel syndrome, the patient must be given ample time to address their sleeping posture and they must also prove that they do not have entrapment of the ulnar nerve at the wrist level; i.e. Guyon's canal. Recurrence may be more likely to occur in a diabetic than a nondiabetic person. Since September 2009 I have been using an endoscopically-assisted technique in all patients who are lean enough to safely perform it and cooperative enough to ensure its success. I have been impressed by the reduction in postoperative bruising and the minimal discomfort noted by my patients as well as the appropriate elimination or improvement of cubital tunnel symptoms. I require confirmation of improved sleep posture to proceed with in-situ endoscopically-assisted ulnar nerve decompression. This provides a significant advantage to the patient with less post-operative discomfort and faster recovery when compared with other surgical techniques.
There are advocates of early surgical treatment of cubital tunnel syndrome, even for patients with negative electrodiagnostic studies because of the good results that may be achieved while avoiding irreversible deformity and disability.
Our Surgical Treatment Recommendations for Cubital Tunnel Syndrome
Endo-Cubital Decompression
Dr. Ichtertz now advocates in-situ endoscopic cubital decompression for the majority of my patients, as long as the patient is cooperative with correcting elbow posture and does not exhibit severe weakness or muscle atrophy. Prior to 2009, however, he had predominantly performed comprehensive decompression of the ulnar nerve through about a 2-inch incision (obese patients require a slightly larger incision for their own protection) which is placed behind the midline of the inner elbow such as to be invisible most of the time. This outpatient surgery is done preferably under a light general anesthetic or a regional supraclavicular nerve block.
Ulnar Transposition
Regardless of the methodology and surgical treatment, there is a broad range of complaints from most people having very little pain to a very few others complaining vociferously of pain lasting anywhere from a few days to more than six months. It is rare to require medication for pain in the elbow beyond a few days at most.
Athletes And Cubital Tunnel Syndrome
For the most part, an athlete needs to be protected from inner elbow instability. My suspicion is that a lot of people who are undergoing "Tommy John" elbow surgery actually have cubital tunnel syndrome and an integral portion of that surgery involves decompression of the ulnar nerve at the elbow. I have never had to reconstruct the inner elbow because of instability developing as a result of cubital tunnel decompression. I do think that it is a good idea to avoid any weakening of the medial elbow ligaments in the throwing arm of a throwing athlete. Therefore perhaps the best method of decompressing an athlete's cubital tunnel is anterior subcutaneous nerve transposition or the in-situ techique. This involves freeing the nerve of overlying constriction and sliding it forward of the medial epicondyle and securing it in the new location.
Anterior Interosseous Nerve Transfer
For treatment of late, severe cubital tunnel with muscle weakness with or without atrophy, the technique, anterior interosseous nerve transfer to the ulnar motor branch at the wrist may be beneficial for a small subset of people that come in with marked weakness in association with cubital tunnel syndrome. If it has just occurred over a very short period and preferably before any muscle wasting has occurred, these individuals may benefit from anterior interosseous nerve transfer into the ulnar motor branch at the wrist. This is a relatively minor operation and can be done as an outpatient. It was invented in the mid-1990’s for severe ulnar nerve injury at the elbow or above because it takes so long for the ulnar nerve to recover and muscles are usually wasted away. The anterior interosseous nerve at the level of the wrist can be sacrificed without any deficit because at that point it only innervates the muscle known as the pronator quadratus which does very little for the forearm. By transferring this nerve into the ulnar nerve motor branch at the wrist, coined “supercharging it”, by Susan McKinnon, MD, plastic surgeon at Washington University in St. Louis, the person has a possibility of gaining recovery of muscle function in the hand innervated by the ulnar nerve because the connection between the transferred anterior interosseous and the ulnar motor branch has such a short healing time. Long term follow up data is as yet lacking on the value of this procedure as promoted by Dr. McKinnon.
Resumption of Activity
A person may resume most of her normal activity within a few days of surgery with the exception of forceful pounding or throwing in the case of a transposition or epicondylectomy. No restriction is required for those undergoing an in- situ procedure. Pounding may not be well tolerated for a few weeks.
Amadio P: “Anatomical basis for a technique of ulnar nerve transposition.” Surg Rad. Anatomy 1986;155-161.
Apfelberg DB, Larson SJ: “Dynamic anatomy of the ulnar nerve at the elbow.” Plastic & Reconstructive Surg. 1973;51: 1:76-81.
Biggs M, Curtis JA: “Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition.” Neurosurgery 2006;58:2:296-303.
Blacker GJ, Lister GD, Kleinert HE: “The abducted little finger in low ulnar nerve palsy.” J Hand Surg 1976;1:3:190-196.
Chung KC: “Treatment of ulnar nerve compression at the elbow.: J Hand Surg 2008;33A:1625-1627.
Craven P, Green D: “Cubital tunnel syndrome: treatment by medial epicondylectomy.” J Bone & Joint Surg 1980;62A:6:980.
Dellon AL, Hament W, Gittelshon A: “Nonoperatvie management of cubital tunnel syndrome: an 8 year prospective study.” Neurology 1993;43:1673-1677.
Dellon AL: “Extensor digiti minimi tendon transfer to correct abducted small finger in ulnar dysfunction.” J Hand Surg 1991;16:5:819-823.
Dimond M, Lister G: “Cubital tunnel syndrome treated by long-arm splintage.” J Hand Surg 1985;10A,430.
Eisen A, Danon J: “The mild cubital tunnel syndrome.” Neurology 1974;24:608-613.
Froimson A, Zahrawi F: “Treatment of neuropathy of the ulnar nerve at the elbow by epicondylectomy and neurolysis.” J Hand Surg 1980;5:391-395.
Gabel G, Morrey B: “Operative treatment of medial epicondylitis.” J Bone & Joint Surg 1995;77A:7:1065.
Gervasio O, Gambardella G, el al “Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: A prospective randomized study.” Neurosurgery 2005; 56:1:108-117.
Geutjens GG, Langstaff RJ, Smith NJ, Jefferson D, Howell, CJ, Baron NJ: “Medial epicondylectomy or ulnar nerve transposition for ulnar neuropathy at the elbow?” J Bone & Joint Surg 1996;78B:6:777.
Hamlin C, Littler W: “Restoration of power pinch.” J Hand Surg 1979;396.
Hastings H II, McCollam SM: “Flexor digitorum superficialis lasso tendon transfer in isolated ulnar nerve palsy: a functional evaluation.” J Hand Surg 1994;19A:275-280.
Jones R, Gauntt C: “Medial epicondylectomy for ulnar nerve compression syndrome at the elbow.” Clinical Ortho 1979;139:174-178.
Kleinmann WB, Bishop AT: “Anterior intramuscular transposition of the ulnar nerve.” J Hand Surg 14A:972-979.
Macnicol MF: “The results of operation for ulnar neuritis.” J Bone & Joint Surg 1979;61B:2:159.
Mansukhani, KA, D’SOuza CD: “Ulnar neuropathy at the elbow in diamond assorters.” Indian J Medical Research 1991;B94:443-436,
Mowlavi A, et al. “The management of cubital tunnel syndrome: A meta-analysis of clinical studies.” Plastic & Reconstructive Surg 2000; 106:2:327-334.
Nabhan A, Ahlehelm F, Reith W, Schwerdtfeger K, Steudel WI: 'Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome.” J Hand Surg 2005;30B:521-524.
Seror P: “Treatment of ulnar nerve palsy at the elbow with night splint.” J Bone & Joint Surg 1993;75B:2:322-327.
Tomaino M, Brach P, Vansickle D: “The rationale for an efficacy of surgical intervention for electrodiagnostic-negative cubital tunnel syndrome.” J Hand Surg 2001;26:1077-1081.
Werner C, Ohlin P, Elmqvist D: “Pressures recorded in ulnar neuropathy.” Acta Orthopaedics Scandinavica 1985;56:404.
Voche P, Merle M: “Wartenberg’s sign: a new method of surgical correction.” J Hand Surg Brit 1995;20B:1:49-52
Witt,J. “Treatment of de Quervain Tenosynovitis: A Prospective Study of the Results of Injection of Steroids and Immobilization in a Splint.” Journal of Bone & Joint Surgery, Vol. 73, 1991, pp. 219-222
Woods, T.H.E., “deQuervain’s disease: a plea for early operation: a report on 40 cases.” British Journal of Surgery, Vol. 51, No. 5, May 1964, pp. 358-359.
The Journal of Hand Surgery: British & European Volume Volume 31, Issue 1, February 2006, Pages 23-29 R. Hoffmann