Torn Rotator Cuff
If you are suffering from a torn rotator cuff, receiving proper medical treatment quickly can affect how well you recover from this injury. At Nebraska Hand & Shoulder, we are not only concerned with repairing your rotator cuff, but we are also committed to returning you to your daily activities as soon as possible. With our advanced surgical procedures, we are able to minimize scarring and reduce your recovery time when compared to traditional surgical methods. Schedule an appointment today to see our expert surgical staff for your torn rotator cuff.
More About Torn Rotator Cuff Injuries
Damage to the rotator cuff has become an increasingly more frequent event. Twenty-eight years or more ago it was seen almost exclusively in the realm of retirees in their late 60s on up. Now we are frequently treating people in their 50s and occasionally their 40s or earlier. In general in the 1980s, there was a big controversy around how to diagnose a torn rotator cuff and many then and before went undiagnosed and people just suffered. In the 1990s, treatments formerly only available through open surgical techniques shifted to arthroscopic techniques with better visualization afforded with the arthroscope; though technically more difficult, new technically demanding procedures and equipment to perform those procedures evolved. In the early 1980s latissimus dorsi and serratus anterior muscles which become very large and bulky and prominent in bodybuilders found extensive use in microvascular reconstructive surgery. Portions of each of these muscles can be taken and moved with its blood vessel and nerve and reattached elsewhere in the body to fill a large void from trauma or tumor resection. This is true without sacrificing function of the shoulder. Since the late 1990s the latissimus dorsi muscle has gained limited use in reconstruction of massive rotator cuff deficiency to help stabilize the shoulder and also to strengthen external rotation.
A torn rotator cuff usually occurs after some vigorous forceful activity including a fall. Those in the older age spectrum frequently can't recall any injury. Whether it is because of poor memory or just the fact that their tendon has been decaying slowly and ultimately just snapped is unclear. It appears that there is some of both occurring. There is certainly much better tissue quality to work on in the person who has a traumatic injury to the rotator cuff rather than the person who seems to have a degenerative spontaneous disruption.
Controversy remains as to what role the overlying acromion has in the majority of patients with a torn rotator cuff. In some patients there is such a prominent bone developing spontaneously that it appears to rub a hole in the rotator cuff. In these same patients a quick forceful action may act somewhat akin to taking scissors across a tightly held piece of cloth resulting in a tear; people that fit into this category typically have an acromion described as "type 3".

Type 3 acromion
WARNING: MAY CONTAIN GRAPHIC IMAGES
Diagnosis
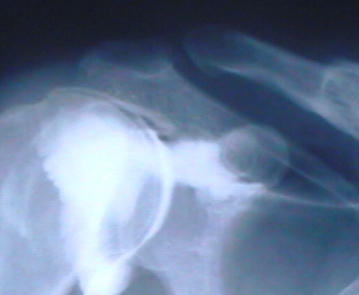
Confirmation of a torn rotator cuff is required for definitive treatment. A person presenting with persistent pain and particularly if there is weakness and associated loss of motion is probably a good candidate for either an arthrogram (dye injected with a sterile needle) or an MRI scan. In the last 10 years MRI has become the diagnostic exam of choice because it is the only test that allows us to not only confirm the presence of a torn tendon, but to get a good idea of how large the tear is and the condition of the muscle. This affects the treatment options, urgency of treatment, and the possibility of treatment. In some cases it could be too large and too old for surgery to benefit the person. This helps set the stage for preparation for both the surgeon and the patient.
An arthrogram is a very useful tool and much less costly. There are a fair percentage of false-positive tests suggesting a torn rotator cuff when, in fact, the tendon is intact. An arthrogram does not allow us to tell the size of a torn rotator cuff and so it is used less these days. It is still a useful tool especially in those with pacemakers, etc. who are not able to have an MRI.
In a combination test, an MRI-arthrogram helps to add a little extra definition in the rare damage to the glenoid labrum. Glenoid labral abnormalities occur very rarely in a fashion such that they are symptomatic. They are commonly identified in the patients undergoing surgery for a torn rotator cuff. In these individuals the pathology of the abnormalities identified in the labrum probably have absolutely nothing to do with the person's complaints and oftentimes can go untreated without the person having ongoing symptoms.
Normal acromion
Timing of Repair
Timing of repair depends a lot on how symptomatic a person is and how healthy the person is. How bad symptoms are relates to the size of the tear and activity level. There is a certain percentage of our population that seems to be oblivious of certain types of problems. A person may harbor a large rotator cuff tear with seemingly no problem, full range of motion, and full strength until some minor injury offsets their balance and precipitates pain. These people are probably best treated just with physical therapy and medication. It is hard to be certain in each case what we are dealing with.
A fresh, large (>3 cm) rotator cuff tear with significant weakness and pain should be treated aggressively and early, preferably within three to six weeks. The longer a person waits in getting repair, the more difficult it makes it for the surgeon. It also decreases the chances of a solid repair and an excellent outcome.
The results of surgery depend on age of the patient and size and configuration of the tear and the timing of the repair; the larger the tear with the older patient, the greater chance that it won't heal completely. Studies have demonstrated only about 75% of really large rotator cuff tears heal, epecially in cases with older patients or those who delay in coming to doctor. Yet between 80% and 90% of people surgically treated for torn rotator cuff, on a non-work-related basis, generally report to get very good to excellent outcomes. In the majority of people that present with a torn rotator cuff, acromioplasty is done both for access to do the repair and because of the belief that prominent acromion has a lot to do with the development of the tear. The predominant feature causing pain may be the prominent bone, not the rotator cuff tendon. Thus, the shape of the acromion and its prominence should never be overlooked when addressing a person with shoulder pain.
Partial-Thickness Tears
I don't really like the term "partial-thickness tears" because generally most of the time the tendons don't really look "torn", they just look "worn". There is a lot of fraying and it doesn't have the robust appearance that normal tendon has. On an MRI scan the tendon looks thinner and it is sometimes hard to discern whether there is a hole straight through it or if it is just within the tissue. There is a raging debate as to whether this should be totally ignored at the level of the tendon with all of the attention given to the overlying bone or whether the thinned portion should be removed (resected) and the remaining edges sewn together and down to the bone. It is a very big commitment to a patient to have a rotator cuff repair because she is tied up in a sling for a minimum of a month and limited in her activity for at least three months. This is not only a practical problem in getting dressed and getting about with activities of daily living (ADLs), but it can be extremely costly limiting a person's ability to produce for her family (farm, construction, etc.). There is also a fair amount of discomfort involved for a few days after surgery.
Another controversy is the risk of a "partial-thickness tear" going on to a "full-thickness tear". I personally think that we are best to treat the patient's prominent bone, i.e. eliminate the impingement syndrome, and monitor the patient because one only has to be off work for a couple of days and regain full motion over a week or so very quickly if we just trim the bone (acromioplasty). The cost in both loss of function and financially is much less with acromioplasty with or without outer collar bone removal for associated acromioclavicular arthritis when compared with other traditional surgical methods.
Work-related
Patients treated under the auspices of worker's compensation in most orthopedic offices across the United States report poor outcomes. In my office, the outcomes have typically been as good as those achieved with the private sector (90% good or excellent) but the work in getting the person there has been much more difficult with a lot more coaxing and prodding of the patient. It is generally believed that this dichotomy is due to psychosocial factors in the person blaming the problem on their job. They may be disgruntled and poorly motivated to return to their regular job and ultimately there is an effect of an impairment rating which some people are looking for to supplement their regular income, the "Dollar Poultice effect". Thus, in reviewing the results of rotator cuff surgery, like any treatment offered to patients who consider themselves "injured workers", we have to scrutinize the results carefully. Thus, there has been a big emphasis on separating out subjective and objective complaints, changes in range of motion or strength vs. pain or loss of function which is subjective, and this applies to the most recently used impairment manual from the AMA Guides for Evaluation of Permanent Impairment, 6th Edition.
Poorly Conceived Treatment
Occasionally a technique for which there was a lot of enthusiasm gets pushed to the wayside because of the limited benefit and high risk (eg, thermal capsulorrhaphy). This was introduced as a way of tightening up capsular laxity and reducing pain. Presumably the heat applied causes local pain and nerve fiber removal. Unfortunately, the heat also kills cartilage cells, often eats up too much capsule and creates a worse problem.