Thumb Arthritis
Suffering from thumb arthritis is not only painful, but can affect your ability to perform simple, every day tasks. Unfortunately this condition affects a significant percentage of women over the age of 40. While there are many treatment options, not all will provide the long-term relief that will improve your quality of life. If you are looking for relief from thumb arthritis, contact the experts at Nebraska Hand & Shoulder today to schedule an appointment.
Introduction To Thumb Arthritis
The thumb must be able to come together to touch the fingers and grasp. The trapeziometacarpal joint (CMC) at the bottom of the thumb is primarily responsible for providing the thumb with the important attributes of mobility and rotation. It is hard to overstate the importance of the thumb and good mobility. Arthritis at the base of the thumb may be a disabling condition. It is the most frequent, significant arthritis of the hand. About 1/3 of women over the age of 40 have some CMC arthritis. Women over the age of 50, however, account for 80-90% of cases requiring treatment.
It's not uncommon for a person who presents with CMC arthritis to have other associated pathology in the hand, which may be contributing to the discomfort. In fact, over half of the patients treated with CMC arthritis are found to have simultaneous carpal tunnel syndrome. Trigger digit and de Quervain's tendonosis are also common in the same person. Arthritis is overwhelmingly degenerative and spontaneous, though a small percentage of patients have the CMC joint damaged by rheumatoid disease. In that case, it's auto immune disease (the body attacking itself). Post-traumatic arthritis after a fracture at the base of the thumb is uncommon.
Untreated degenerative arthritis of the thumb CMC joint may result in contracture of the first web space, i.e. the thumb ends up lying closer to the index metacarpal, making it more difficult to open the hand to pinch and grasp objects. Simultaneously, the next joint toward the tip of the thumb (metacarpophalangeal or MP joint) gets stretched out, resulting in hyperextension, impairing grip and pinch. This ultimately results in a "swan neck" type of deformity of the thumb.

X-ray depicting swan neck deformity. Note how the thumb and index metacarpals are pressed tightly together

Contracture of the first web space (the thumb ends up lying closer to the index metacarpal)

Contracture of the first web space & MP joint hyperextended (swan neck deformity)
Symptoms
The person with CMC arthritis usually complains of pain at the base of the thumb or the thumb side of the wrist, especially with motion and pinching. The pain may radiate upwards into the forearm. Difficulty pulling up stockings, opening car doors and jars and trouble turning keys are frequently noted. She often drops things due to the weakness associated with the discomfort or loss of dexterity due to carpal tunnel syndrome. Usually by the time she presents to a doctor, there is also a visible and palpable (can feel with opposite hand) enlargement over the base of the CMC related to new bone formation and joint slippage (subluxation). Numbness, awakening at night due to pain, and clumsiness also suggest carpal tunnel syndrome is present.

Enlargement at the base of the thumb
Diagnosis
When a person is seen with pain at the base of the thumb, the doctor must go through a differential diagnosis to exclude de Quervain's tendonitis, trigger thumb, and carpal tunnel syndrome. Physical examination should include the grind test (pushing the end of the thumb towards the wrist and rotation in a pestle and mortar fashion in an attempt to cause pain and grating), the doctor also looks for localized tenderness, measures joint range of motion and grip and pinch strength. X-rays of the wrist are also used to confirm and stage the extent of the arthritis.
Nerve conduction study is usually indicated to evaluate for median nerve entrapment at the carpal tunnel. An unrelieved carpal tunnel may result in a return to the operating room if not detected preoperatively. Research has shown that over half of the people who present with arthritis at the base of the thumb have median nerve entrapment simultaneously. It is not known whether this is a cause and effect.
Treatment Goals
- Pain relief
- Strong, functional grip and pinch
- Normal thumb mobility
- Improved appearance
Non-Operative Treatment
Once a diagnosis is established, if there are no reasons to avoid using oral anti-inflammatory medications (NSAID) such as ulcer disease, gastritis, esophagitis, long-term anti-coagulation or allergies- a trial of nonsteroidal anti-inflammatory medication and/or acetaminophen (Tylenol) may be given. The most common examples of NSAIDs are meloxicam (once a day), Celebrex (twice a day), naproxen sodium (twice a day), diclofenac (twice a day), topical 1% Voltaren gel (compounded, alcohol-based), and topical ketoprofen 20% cream. One needs to use these for at least 3 weeks before giving up. This does not solve the underlying problem but may eliminate the symptoms in the wrist if taken on a regular basis.
- NSAIDS
- Cortisone injections
- Braces
Alternatively, cortisone injection into the CMC joint may give temporary symptomatic relief. The injection hurts but it may be offered to the person making up her mind with regard to the various options. Cortisone injection for this purpose is extremely safe but often hurts to give. An occasional person may experience a temporary flare of pain lasting about a day. Hyaluronic acid (rooster comb) injection, eg: Euflexxa, Synvisc etc. has limited benefit for arthritic knees but does not work for wrist arthritis any better than cortisone. Cortisone is much less expensive. Splinting may provide some relief if the person doesn't use her hand very much. However, splints tend to be bulky and get in the way of function and hygiene. If arthritis symptoms persist in the thumb despite these options, definitive surgery is available for lasting relief.
Surgical Treatment
Surgery is usually done under regional anesthesia by numbing from the hand to the shoulder or general anesthesia as an outpatient. Surgical treatment of CMC arthritis has evolved over the past 60 years and can be generally categorized into 4 different options:
- Resection arthroplasty (with or without TightRope suspension)
- Implant arthroplasty (titanium or pyrocarbon)
- Metacarpal osteotomy
- Fusion

X-Ray Before Tight Rope Suspension Surgery

X-Ray After Tight Rope Suspension Surgery

X-Ray of a Pyrocarbon Implant
WARNING: MAY CONTAIN GRAPHIC IMAGES
Numerous studies have been done to determine the best surgical option. Resection arthroplasty appears to be the best choice for the majority of patients who require surgical treatment. Removal of either part or the entire trapezium depends upon whether the person has arthritis on both sides of this joint or simply one side. Resection arthroplasty results in a pain-free, stable thumb. This is achieved without inserting foreign material such as silicone. Studies comparing patients who have undergone silicone arthroplasty (plastic joint) and those undergoing resection arthroplasty fail to demonstrate any significant functional differences in the two. Resection arthroplasty was introduced in 1948. Resection arthroplasty is usually performed with a tendon used as a cushion. The arthritis usually requires removal of the entire trapezium. The void from the removed bone is filled by a rolled up tendon. The metacarpal is suspended by the intermetacarpal ligament. For arthritis limited to the trapeziometacarpal joint (rather than both sides of the trapezium), titanium or pyrocarbon hemi-arthroplasty are sometimes a good option.
Arthroscopic Resection
A method for arthroscopic resection of the trapezium was also developed over 20 years ago. Results are comparable to those of the formal open procedure. Using the added technology necessary for arthroscopy does add to operative time and cost, and thus the small gain from the smaller incision has to be carefully weighed as the 3 week recovery time spent wearing a brace has not been reduced.
Treatment of Thumb MP Joint Hyperextension Deformity
In advanced cases of CMC joint arthritis, by the time the person presents for treatment the palmar plate of the adjacent MP joint has been substantially stretched out. This occurs to accommodate protective self-splinting and results in web space contracture. To get the best use of the thumb and best appearance with the reconstruction, this abnormal alignment of the thumb MP joint may need to be corrected. There are about 3 ways of addressing this. They all involve a small incision on the palmar aspect of the thumb MP joint and tether either the palmar plate in a more tight position or advance the small thumb muscle (flexor pollicis brevis). This requires additional temporary pin placement across the MP joint that needs to be removed between four and six weeks after the surgery. At least an additional two weeks of post-operative immobilization allows the tissue to heal enough so that it doesn't stretch out. Despite this maneuver, a small percentage of the people who go on to require this in the first place end up stretching out the MP "capsulodesis" reversing some of the benefit. To minimize this Dr. Ichtertz creates a longitudinal scar to reinforce the capsulodesis. The best results are achieved in patients who maintain the corrected alignment.

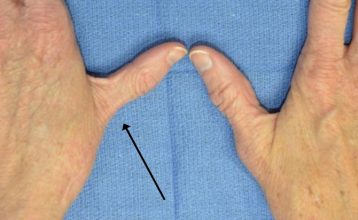
Example of MP joint hyperextension
Post-Operative Management
Most people have soreness for a few days post-op. This is minimized by keeping the hand above the heart continuously for the first week post-op to reduce pain, swelling and prevent stiffness. A lightweight splint is worn for about 3 weeks in the majority of patients while those requiring a pin to stabilize the MP joint or the base of the thumb- in selected cases- will be protected for 6 weeks. Thumb range of motion exercises are begun at 1 to 3 weeks in those not requiring a pin placement. The pin is left hidden under the skin. It needs to be removed under local anesthesia between 4 and 6 weeks post-op. Resistive exercises to regain strength are begun at 3 weeks and 6 weeks, respectively.
Rehabilitation
Motion is generally recovered within a few days of discontinuing the splint. The main goal that is worked on after discontinuing of the post-operative splint is regaining one's pinch and grip strength. Exercises 3 or more times per day with TheraPutty are important. TheraPutty comes color-coded for multiple resistances- we usually use red, which is intermediate. In addition, particularly for gaining strength, the common household spring-loaded toilet paper holder is an excellent device for helping to build up pinch strength. Most people undergoing this surgery obtain complete pain relief and improvement in their pinch strength.

TheraPutty Exercises

Spring-Loaded Toilet Paper Holder Exercises
Fusion of the CMC
This technique is not frequently used. Fusion means to bond one bone to the other so that there is no motion of the joint. Upon fusing the thumb CMC, a person is unable to lay her palm flat, thus it is felt by some to result in an awkward restriction of motion. Additionally, failure of the fusion to unite- especially a problem with smokers- may require additional surgery in order to affect bone union. During the course of healing over 3 to 4 months, the patient has to wear a brace or cast. Additionally, for a person with arthritis on both sides of the trapezium, which is quite frequent, she would not have the option of fusion because it would entail almost fusing the entire wrist.
Osteotomy
Surgically breaking the metacarpal bone just above the joint has been reported to have good pain relief results in the majority of patients. Exactly how pain is reduced with this technique is uncertain. There is no need for foreign material that might result in a reaction such as silicone or implant loosening. This procedure is particularly suited for an individual with marked web space contracture wherein the thumb metacarpal is pulled against the index. However, this procedure does not result in improved range of motion because nothing is done directly to the arthritic CMC joint. There is also additional time necessary for bone healing at the osteotomy site, not a necessity when resection arthroplasty or implant arthroplasty are performed.
Total Joint Arthroplasty
Complete replacement of the thumb CMC joint, similar to total knee replacement, is a difficult procedure with disappointing results in most surgeon's hands. In contrast with joint replacement of larger joints such as the hip or knee, there is little bone with which to secure fixation of the implant. Because of the heavy force the thumb is subjected to, there appears to be a higher rate of loosening. With loosening comes pain and then removal of the implant, i.e. back to the starting point. Thus, total joint replacement of the CMC joint of the thumb is generally not considered a surgical option at this time.
Risks of surgery
Any surgery on the base of the thumb includes a risk of temporary numbness, a very small risk of permanent numbness, or hypersensitivity from injury to superficial nerves. There is about a 1 in 200 chance of infection. Blood loss is minimal. Only implant arthroplasty is associated with dislocation and possible foreign body reaction, such as silicone synovitis. A small change in measurable pinch strength occurs but is outweighed by elimination of pain. However, patients rarely perceive weakness once fully healed. Occasionally the base of the thumb ends up being mildly enlarged or puffy. This probably relates to scar and subtle settling of the thumb and can't be helped. It does not affect pain relief or function.
Results of Resection Arthroplasty
As noted below, marked relief of pain and restoration of function and motion are achieved in the majority of patients treated with CMC arthroplasty.
- P. Amadio, M.D. in 1982 reported 94% satisfaction
- R. Burton, M.D. in 1986 reported 92% satisfaction
- J. Menson, M.D. in 1981 reported 96% satisfaction
- A. Swanson, M.D. in 1997 reported 97% satisfaction
Which Do You Prefer?

This patient has had surgery on the right thumb. Notice how the left thumb is still deformed?
Amadio P, Millender L, Smith R: Silicone spacer or tendon spacer for trapezium resection arthroplasty -comparison of results. J Hand Surg 1982; 7:237.
Calandruccio J, Jobe R: Arthroplasty of the thumb carpometacarpal joint. Seminars in Arthroplasty 1997: 135-147.
Badger E: Arthrodesis of the carpometacarpal joint of the thumb. J Bone Joint Surg 1964; 46B:16.
Bunnell S: Surgery of the Hand: 3rd Edition, Philadelphia J.B. Lippincott Co. 1956; 823.
Bossley CJ: Basal osteotomy of the first metacarpal for osteoarthritis of the first carpal metacarpal joint. J Bone Joint Surg 1981; 63B:468.
Brase DW, Millander LH: Failure of silicone rubber wrist arthroplasty in rheumatoid arthritis. J Hand Surg 1986; 1A:175.
Burton R, Pellegrini VD: Surgical management of basal joint arthritis of the thumb Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg 1986; 11A:324.
Carroll RE, Hill NA: Arthrodesis of the carpometacarpal joint of the thumb. J Bone Surg 1973; 55B:292.
Carter PR, Benton LJ, Dysert PA: Silicone rubber carpal implants: a study of the incidence of late osseous complications. J Hand Surg 1986; 11A:639.
Dell PC, Brushart TM, Smith RJ: Treatment of trapeziometacarpal arthritis: results of resection arthroplasty. J Hand Surg 1978; 3:243.
Eaton RG: Replacement of the trapezium for arthritis of the basal articulations. A new technique with stabilization of tenodesis. J Bone Joint Surg 1979; 61A:76.
Eaton RG, Glickel SZ, Littler JW: Tendon interposition arthroplasty for degenerative arthritis of the trapeziometacarpal joint of the thumb. J Hand Surg 1985; 10A:645.
Eaton RG, Littler JW: A study of the basal joint of the thumb: treatment of its disabilities by fusion. J Bone Joint Surg 1969; 51A:661.
Eiken O, Carstam N: Functional assessment of basal joint fusion of the thumb. Scand J Plast Rec Surg 1983; 53:219.
Florack T et al: The prevalence of carpal tunnel syndrome in patients with basal joint arthritis of the thumb. J Hand Surg 1992; 17A:624-630.
Gervis WH: Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint. J Bone Joint Surg 1949: 31B:540.
Gervis WH: A review of excision of the trapezium for osteoarthritis of the trapeziometacarpal joint after twenty-five years. J Bone Joint Surg 1973; 55B:56.
Gordon ML, Bullough PG: Synovial and osseous inflammation in failed silicone rubber prostheses. J Bone Joint Surg 1982; 64A:574.
Graber-Duvernay JB, Graber-Duvernay JL: Remarques sur la rhizarthrose du pouce (d’apres 500 observations). Rev Lyon Med 1970; 19:209.
Haffajee D: Endoprosthetic replacement of the trapezium for arthrosis of the carpometacarpal joint of the thumb. J Hand Surg 1977; 2:141-148.
Haraldsson S: Extirpation of the trapezium for osteoarthritis of the first carpometacarpal joint of the thumb. Acta Orthop Scand 1972; 43:347.
Iyer KM: The results of excision of the trapezium: 26 cases of excisional arthroplasty. Hand 1981; 3:246.
Menon J, Schoene HR, Hohl JC: Trapeziometacarpal arthritis. Results of tendon interpositional arthroplasty. J Hand Surg 1981; 6:442-446.
Murley AH: Excision of the trapezium in osteoarthritis of the first carpal metacarpal joint. J Bone Joint Surg 1960; 42B:502.
Pallegrini V, Burton R: Surgical management of basal joint arthritis of the thumb. Part 1: Long-term results of silicone implant arthroplasty. J Hand Surg 1986; 11A.
Swanson A: Trapezium implant arthroplasty. J Hand Surg 1981; 6A:125-141.
Swanson A, Swanson G, DeHeer D, Pierce T, Randall K, Smith J, VanGorp C: Carpal bone titanium implant arthroplasty. Clinical Ortho 1997; 342:46-58.
Thompson TC: Surgical treatment of trapeziometacarpal arthrosis. Advances in Ortho Surg 1986; 105-120.
Varley GW, et al: Excision of the trapezium for osteoarthritis at the base of the thumb. J Bone Joint Surg ;76B,6; 964-968.
Weilby A, Sondorf J: Results following removal of silicone trapezium metacarpal implants. J Hand Surg 1978; 3:154.
Wilson JN: Basal osteotomy of the first metacarpal in the treatment of arthritis of the carpometacarpal of the thumb. British J Surg 1973; 60:854-58.
Wilson JN, Bossley CJ: Osteotomy in the treatment of osteoarthritis of the first carpal metacarpal joint. J Bone Joint Surg 1983; 65B, 2:179-181.